
Postpartum Depression: What New Mothers in India Need to Know
May 12, 2025
|
18
min read
|
Tanvi


The Other Side of Motherhood
Motherhood is often celebrated as a time of unmatched joy and fulfillment. From baby showers to blessings, the arrival of a newborn is expected to bring happiness. But for many mothers, especially in the weeks and months following childbirth, this period is marked not by joy - but by overwhelming sadness, anxiety, and emotional exhaustion.
This emotional struggle has a name: Postpartum Depression (PPD).
According to the American Psychological Association (APA), postpartum depression is a serious mental health condition that can occur days, weeks, or even months after childbirth, and if left untreated, may last for many weeks or months. It goes far beyond the “baby blues,” affecting a mother’s mood, energy, and ability to care for herself or her baby.
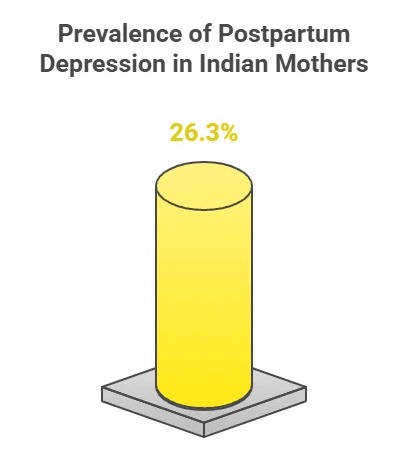
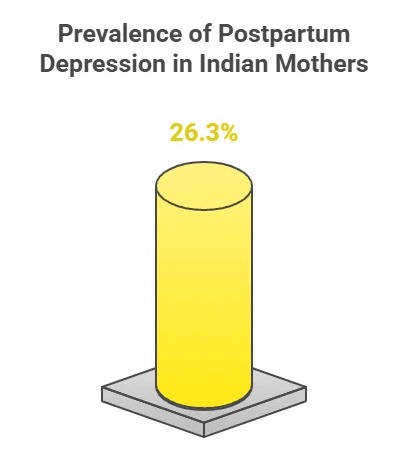
In India, postpartum depression is far more common than many realize. A study by Lanjewar, Shraddha et al. found that 26.3% of Indian mothers experience symptoms of depression after delivery. Despite this high number, cultural stigma, lack of awareness, and limited access to mental health care often prevent mothers from speaking up or seeking help.
What’s more alarming is that for 36% of mothers who experience mental health challenges soon after childbirth, symptoms can persist for as long as 18 months - and in some cases, up to two years. These extended struggles can deeply impact not only the mother’s well-being but also her relationship with her baby, her partner, and herself.
The good news? Postpartum depression is treatable. With the right support, healing is possible.
This blog is here to break the silence. We’ll help you understand what PPD is, how it differs from the baby blues, what signs to look out for, and most importantly - how compassionate, expert-led care like the kind offered by Elfina Health can make a real difference.
Perinatal vs Postpartum Depression vs Prenatal Depression
Motherhood is often described as a beautiful journey - but for many women, it can come with emotional storms that are difficult to explain or share. Understanding the terms used to describe mental health conditions around childbirth is an important first step in recognizing and seeking help.
Perinatal depression is a broad term that includes both prenatal depression (depression during pregnancy) and postpartum depression (depression after childbirth). While the experiences overlap, each phase comes with its own emotional, physical, and psychological challenges.
Definitions and Differences
Term | Timing | Description |
Perinatal Depression | During pregnancy and up to 1 year after birth | An umbrella term for mood disorders before and after childbirth. |
Prenatal Depression | During pregnancy | Depression that occurs during pregnancy - often marked by sadness, fear, or exhaustion. |
Postpartum Depression | After childbirth (typically within 4 weeks to 1 year) | Depression that follows childbirth; more persistent and intense than the "baby blues". |
While these conditions differ in timing, they often share common symptoms like deep sadness, irritability, anxiety, disrupted sleep, and changes in appetite. Unfortunately, they’re frequently overlooked or misunderstood - especially in India - due to social stigma and a lack of mental health awareness.
What Happens During Perinatal Depression?
Perinatal depression is more than just feeling overwhelmed - it's a serious and often misunderstood medical condition. It can affect a mother during pregnancy (prenatal) or after delivery (postpartum), showing up as intense sadness, detachment, anxiety, and drastic changes in energy, appetite, or sleep patterns.
In the case of postpartum depression (PPD), symptoms often appear between the second and sixth week after childbirth, but can develop any time within the first year. While many new mothers experience what’s commonly called the “baby blues,” postpartum depression goes far deeper and lasts much longer. It may involve constant low mood, hopelessness, tearfulness, and even disturbing thoughts - such as excessive worries about the baby's health, feelings of worthlessness, or in extreme cases, suicidal ideation or thoughts of harming the child. These are deeply distressing experiences, and contrary to common belief, they are not signs of being a “bad mother”.
Perinatal depression affects more than just the mother’s mood. It can interfere with her ability to bond with her baby, leading to emotional distance or feelings of guilt and disconnection. According to the APA, perinatal depression can contribute to sleep and feeding difficulties in the baby, creating a stressful environment for both mother and child.
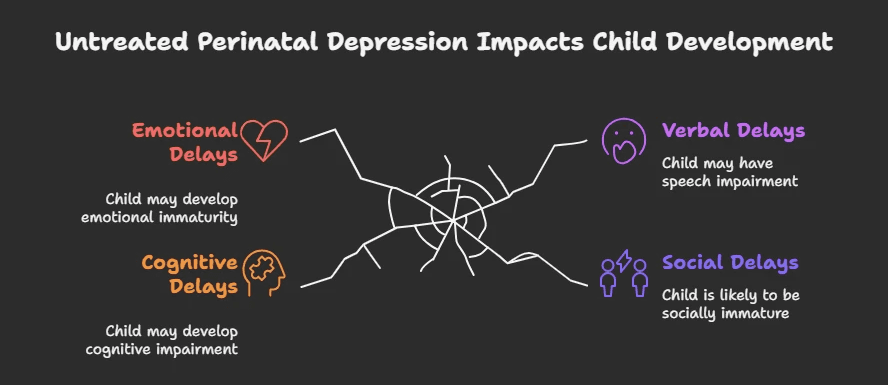
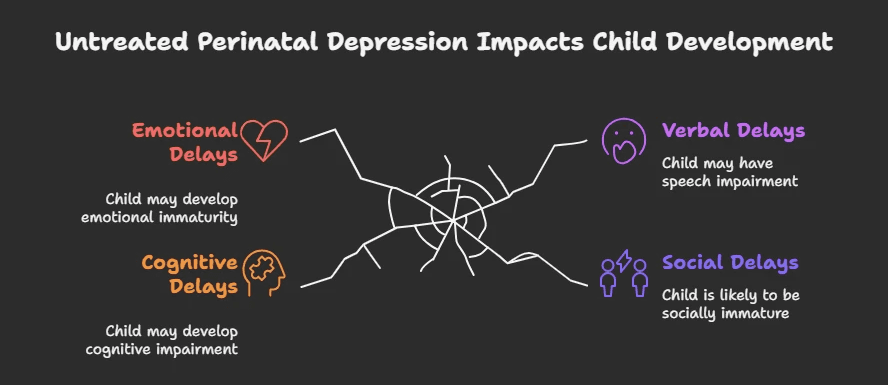
The ripple effects of perinatal depression can be long-term, especially for the child. Research shows that children born to mothers with untreated perinatal depression are at greater risk for cognitive, emotional, verbal, and social developmental delays. Emotional availability in those early stages is crucial for a child’s growth, and when maternal mental health suffers, it can impact the child’s emotional security, attachment, and ability to regulate emotions. These outcomes are not signs of poor parenting - they are the result of an untreated medical condition that deserves timely recognition, compassion, and support.
The good news is that perinatal and postpartum depression are treatable. With the right help - whether through therapy, support groups, medical guidance, or simply being heard - recovery is entirely possible. Early intervention doesn’t just help the mother heal; it also lays a stronger emotional foundation for the child.
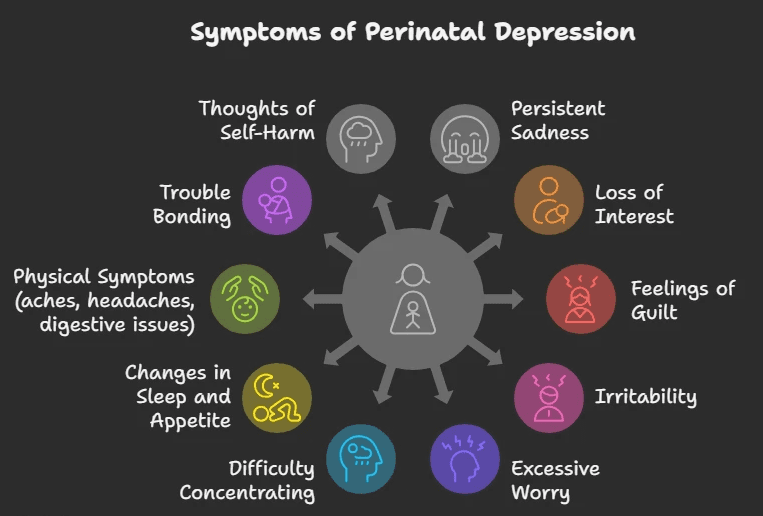
Recognizing the Symptoms of Postpartum Depression
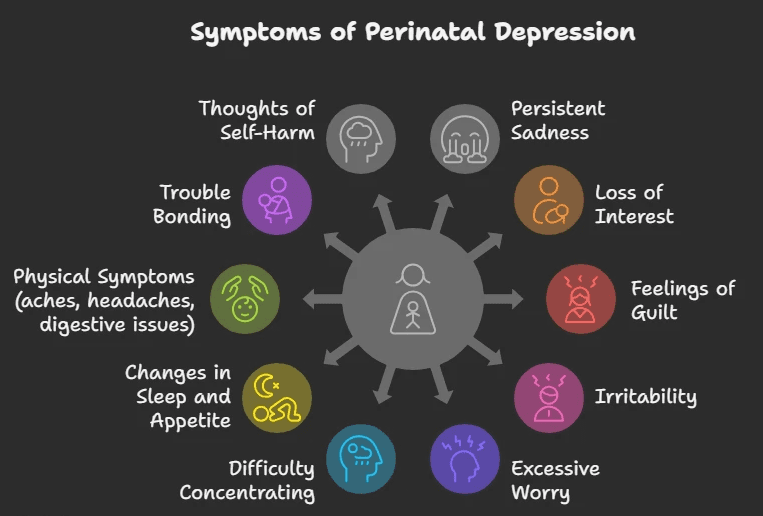
Postpartum Depression doesn’t always look the same for every mother - but it’s more than just feeling tired or overwhelmed. It can manifest emotionally, physically, and behaviorally, often lasting for weeks or even months if left unaddressed.
According to the U.S. National Institute of Mental Health, common symptoms include:
Persistent sadness, anxiety, or a sense of emotional numbness
Many mothers report feeling hopeless or emotionally disconnected most of the day, nearly every day.Loss of interest or joy in activities
This includes disinterest in the baby or things that once brought happiness.Feelings of guilt, worthlessness, or inadequacy
Mothers may blame themselves unnecessarily or feel like they’re failing, even when they’re doing their best.Irritability, restlessness, or frequent frustration
Small things may trigger intense emotions or sudden outbursts.Excessive worry or panic attacks
These may include racing thoughts, heart palpitations, or overwhelming anxiety about the baby’s safety or one’s ability to care for them.Difficulty concentrating or making decisions
A foggy mind or forgetfulness can interfere with daily tasks and responsibilities.Changes in sleep and appetite
This might include insomnia despite exhaustion, sleeping too much, loss of appetite, or overeating.Physical symptoms without a clear cause
Aches, pains, headaches, or digestive issues that don’t respond to usual treatment can be signs.Trouble bonding with the baby
Some mothers feel detached or worry that they aren’t connecting emotionally with their child.Thoughts of self-harm or harming the baby (in severe cases)
These intrusive thoughts can be deeply distressing and are a clear sign to seek immediate professional support.
If you notice these symptoms persisting for more than two weeks, it's important to seek professional help. Postpartum depression is not a personal weakness - it's a medical condition, and with the right support, it can be treated.
Elfina offers confidential, culturally sensitive online counseling tailored for new and expecting mothers.
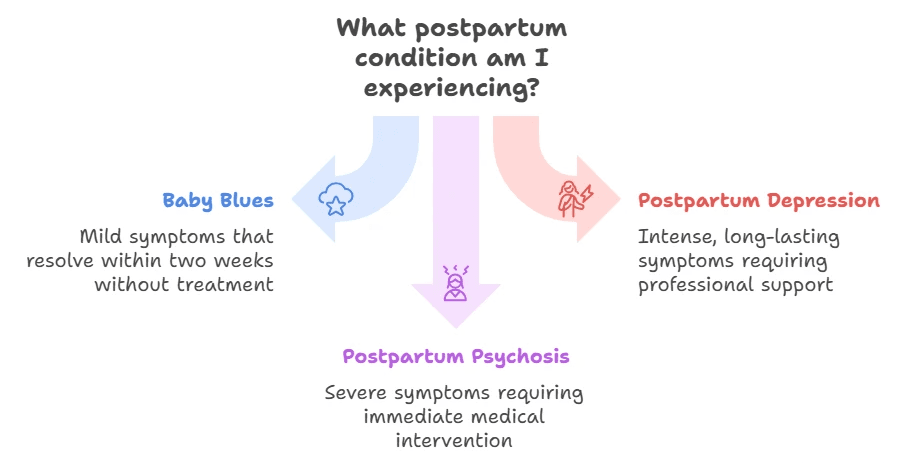
Baby Blues vs Postpartum Depression vs Postpartum Psychosis
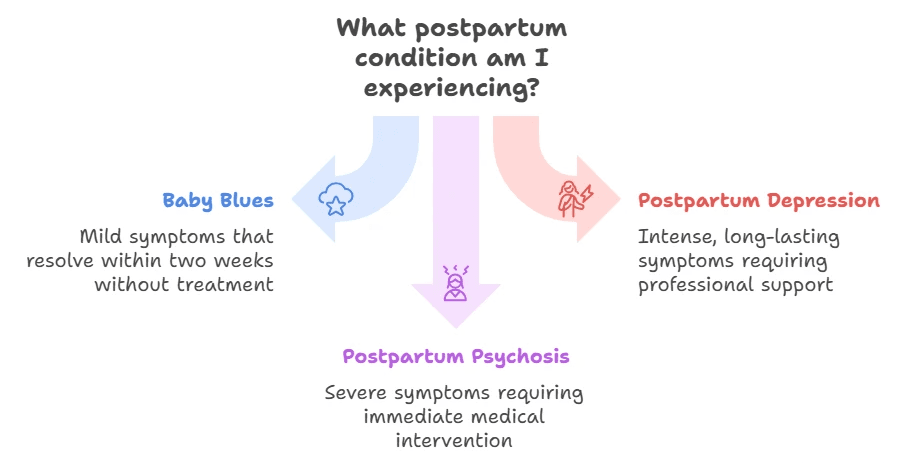
Baby Blues
According to the South Dakota Department of Health, it affects around 70 - 80% of new mothers, often within the first few days after childbirth. Symptoms include mood swings, tearfulness, irritability, and anxiety. These emotional ups and downs are usually mild and tend to resolve on their own within two weeks without medical treatment.
Postpartum Depression (PPD)
Unlike the baby blues, PPD is more intense and long-lasting. It can begin anytime within the first year after delivery, often requiring professional support. Mothers may experience overwhelming sadness, fatigue, hopelessness, loss of interest in the baby, and even thoughts of self-harm. It affects daily functioning and emotional connection with the baby - but it is treatable with the right care.
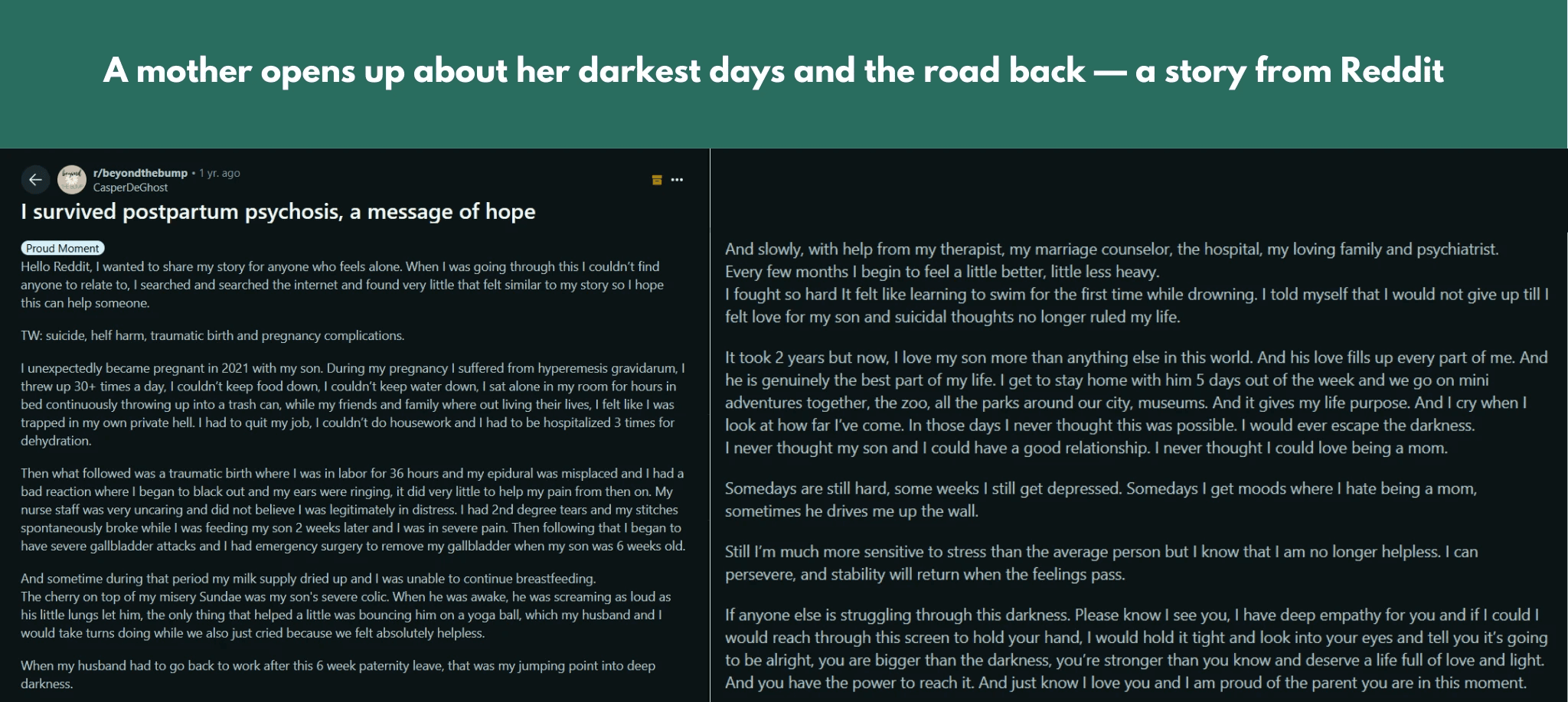
Postpartum Psychosis
A rare but severe condition, postpartum psychosis is a psychiatric emergency that usually develops within the first few days to weeks after childbirth. Symptoms may include hallucinations, delusions, extreme confusion, and disorganized behavior. Immediate medical intervention is critical.
Certain factors such as advanced maternal age and low birth weight (under 1500 grams) are potential contributors, while high birth weight (over 4500 grams) and maternal diabetes may offer some protective effect for first-time mothers within the first 90 days.
Edinburgh Postnatal Depression Scale (EPDS)
The Edinburgh Postnatal Depression Scale (EPDS) is a widely used screening tool designed to help healthcare providers identify mothers who may be experiencing postpartum depression (PPD). It consists of 10 simple, self-reported questions that focus on the emotional state of new mothers, helping to assess feelings such as sadness, hopelessness, and anxiety over the previous week.
For further credibility, you can refer to the full citation:
Cox, J L et al. “Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale.” The British journal of psychiatry : the journal of mental science vol. 150 (1987): 782-6. doi: 10.1192/bjp.150.6.782
We’ve listed the questions below along with the scoring scale to help you evaluate your emotional well-being. It’s important to answer honestly, as this will help determine if you may need further support or intervention.
EDPS Questionnaire
I have been able to laugh and see the funny side of things
0 = As much as I always could
1 = Not quite so much now
2 = Definitely not so much now
3 = Not at all
I have looked forward with enjoyment to things
0 = As much as I ever did
1 = Rather less than I used to
2 = Definitely less than I used to
3 = Hardly at all
I have blamed myself unnecessarily when things went wrong
0 = No, never
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
I have been anxious or worried for no good reason
0 = No, not at all
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
I have felt scared or panicked for no good reason
0 = No, not at all
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
Things have been getting on top of me
0 = No, never
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
I have been so unhappy that I have had difficulty sleeping
0 = No, never
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, most of the time
I have felt sad or miserable
0 = No, never
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
I have been so unhappy that I have been crying
0 = No, never
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
The thought of harming myself has occurred to me
0 = No, never
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
📊 EPDS Scoring Guide
Here’s the EDPS Scoring Guide as per COPE (Centre of Perinatal Excellence):
🔢 Total Score:
13 or more → 🟠 Possible Depressive Symptoms
This score signals the need for follow-up.
Antenatal period: Repeat the EPDS in 2–4 weeks. If the second score remains ≥13, refer to an appropriate health professional, preferably the woman's general practitioner.
Postnatal period: Consider referral or continued care based on clinical judgment.
💬 Questions 3, 4, and 5 → ⚠️ Monitor for Anxiety
Even if the total score is below 13, elevated responses on these questions may indicate anxiety symptoms requiring follow-up.
🔴 Question 10 (Self-harm)
If the response is 1, 2, or 3, it’s critical to assess the safety of the woman and any children in her care. Seek urgent advice and/or arrange a mental health assessment based on clinical judgment.
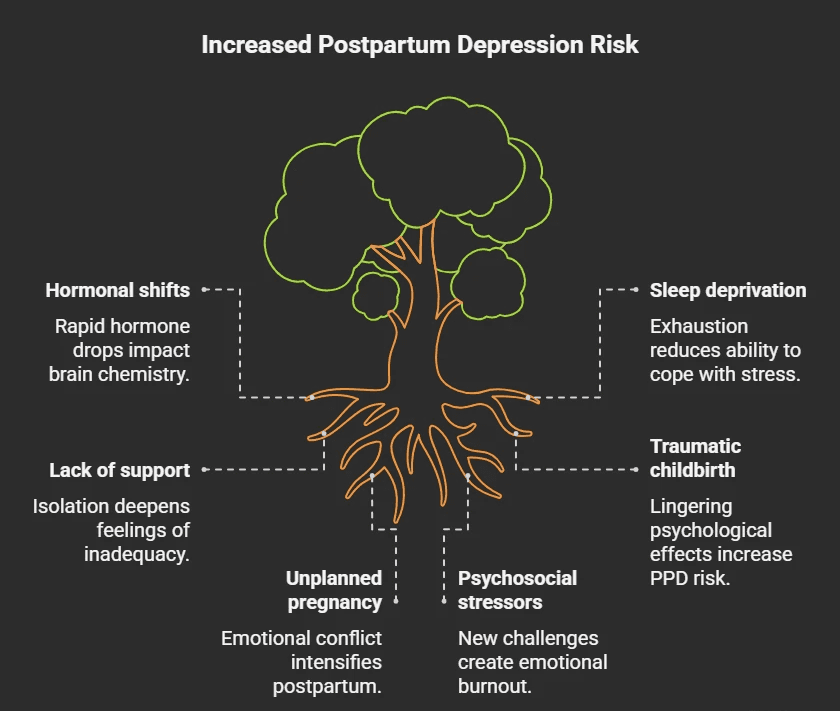
🧠 What Causes Postpartum Depression (PPD)?
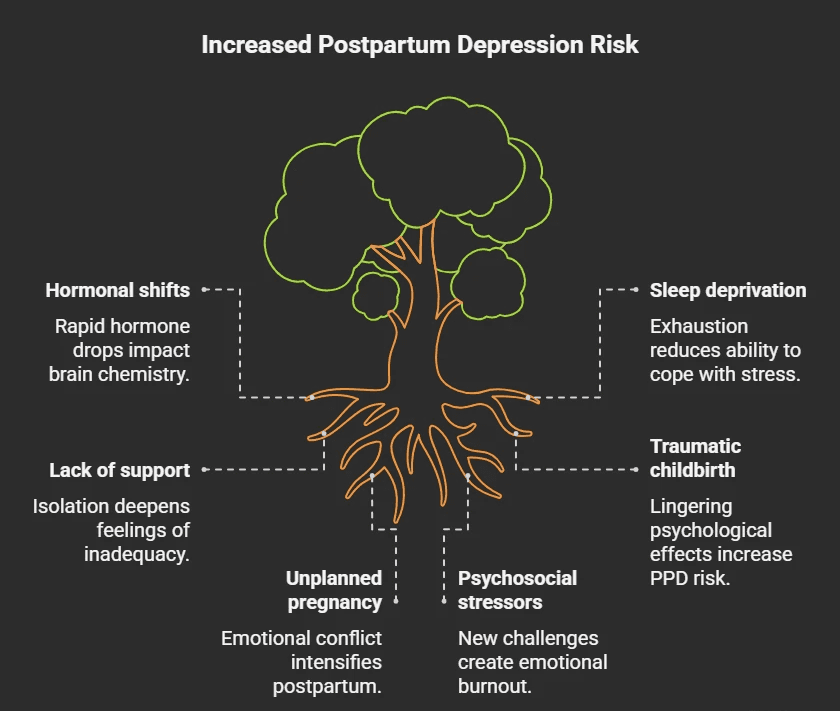
Postpartum Depression (PPD) doesn’t stem from a single cause - it’s the result of a complex interplay between hormonal, emotional, physical, and environmental factors. While every new parent’s journey is different, certain experiences and conditions can significantly increase the risk.
🔄 Hormonal Fluctuations
After childbirth, estrogen and progesterone levels - which were elevated throughout pregnancy - drop sharply. These rapid hormonal shifts can impact brain chemistry and trigger mood disturbances, especially in individuals already sensitive to such changes.
😴 Sleep Deprivation & Physical Exhaustion
Caring for a newborn often means interrupted or inadequate sleep, which can compound physical fatigue and emotional instability. Prolonged exhaustion not only affects mood but also limits one’s ability to cope with daily stressors, increasing vulnerability to depression.
💔 Lack of Emotional or Social Support
Feeling unsupported - whether by a partner, family, friends, or community - can deepen feelings of isolation, inadequacy, or helplessness. Emotional availability from others plays a crucial role in helping new parents adjust and feel seen during this transition.
🚨 Traumatic Childbirth
Difficult or traumatic birth experiences - such as emergency C-sections, excessive pain, complications, or feeling a loss of control - can have lingering psychological effects. These may include flashbacks, heightened anxiety, and an increased risk of PPD, anxiety disorders, or even postpartum psychosis.
🤰 Unplanned or Unintended Pregnancy
Pregnancies that were unplanned - even if not unwelcome - can contribute to emotional conflict, stress, or ambivalence. These feelings may intensify postpartum, especially in the absence of adequate preparation or support.
🌀 Psychosocial Stressors
The postpartum period is filled with new challenges: identity shifts, physical recovery, lifestyle changes, financial strain, and a redefinition of relationships. When these are combined with unrealistic societal expectations or self-imposed pressure to "bounce back", it can create a perfect storm for emotional burnout.
Even though these causes may raise the risk, PPD can affect anyone - regardless of how “prepared” or “happy” they felt about the pregnancy. Recognizing these risk factors helps reduce stigma and encourages early, compassionate support.
⚠️ Risk Factors for Postpartum Depression
While anyone can experience PPD, certain circumstances may increase the likelihood of its onset. These risk factors span physical, psychological, cultural, and environmental domains:
👶 First-Time Motherhood
Navigating the unknowns of parenting for the first time can bring anxiety, insecurity, and overwhelming responsibility - especially without prior experience or adequate guidance.
🧠 Personal or Family History of Mental Illness
Individuals with a history of depression, anxiety, bipolar disorder, or schizophrenia - or those with close family members who’ve experienced such conditions - are at a higher risk for developing PPD.
💔 Financial, Relationship, or Marital Stress
Tensions around money, unstable partnerships, or unresolved conflicts can place an emotional strain during what should be a time of recovery and bonding.
🏥 Birth or Breastfeeding Complications
Experiencing a traumatic labor, emergency C-section, preterm delivery, difficulty breastfeeding, or a low-birth-weight baby can increase stress and feelings of inadequacy or failure.
🧍 Limited Social or Emotional Support
Lack of involvement or understanding from a partner, family, or community can intensify feelings of isolation - especially in cultures where motherhood is idealized and support is minimal.
🌙 Postpartum Sleep Disruption
Severe sleep deprivation or irregular sleep patterns during the postpartum period not only affect physical health but can dramatically worsen mood and cognitive functioning.
⚖️ Obesity and Nutritional Factors
Studies indicate a positive correlation between higher levels of obesity and PPD risk. Nutritional deficiencies - such as low Vitamin D or iron (postpartum anemia) - may also play a role.
🚼 Cultural Pressures and Gender Preference
In some societies, particularly in parts of Asia and Africa, giving birth to a female child may lead to social pressure or disappointment, exacerbating emotional distress for new mothers.
🧍♀️ Multiple Births or Preterm Infants
Managing twins or more, or caring for premature or medically fragile babies, requires heightened attention and resources - often leading to exhaustion and emotional strain.
💬 If you recognize yourself in any of these risk factors or feel overwhelmed during your postpartum journey, know that you're not alone. Early awareness can make a world of difference. At Elfina, our experts are here to support you with compassionate, culturally sensitive, and evidence-based guidance. Whether it’s your first baby or not, reaching out for help is a powerful act of care - for yourself and your child.
🧡 Don’t wait for things to get worse - connect with Elfina early for personalized support.
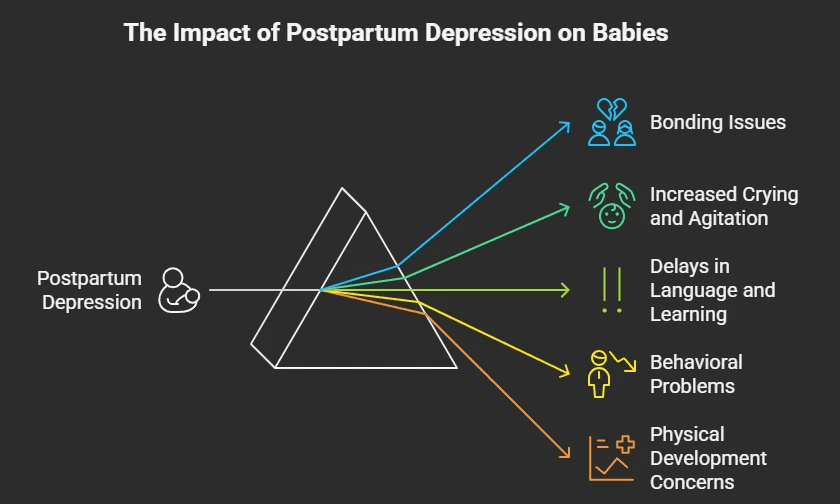
Can Postpartum Depression Affect the Baby?
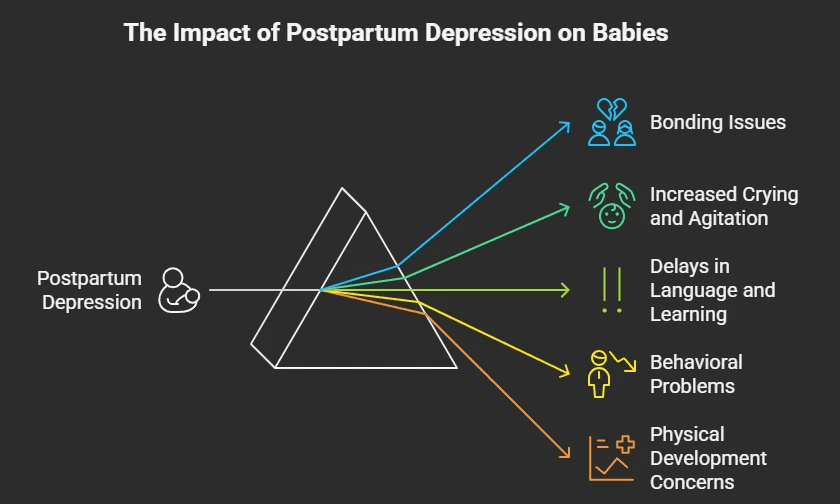
The U.S. Office on Women’s Health compiled leading research on how postpartum depression (PPD) can affect babies - and the findings show it can have a real and lasting impact if left untreated:
🧸 Bonding issues: PPD can make it difficult for mothers to connect emotionally with their babies, leading to attachment problems.
😢 Increased crying and agitation: Babies may cry more often and seem harder to soothe.
🧠 Delays in language and learning: Children may take longer to start speaking or have trouble with early learning.
🚸 Behavioral problems: These can include trouble adjusting to school or new environments, as well as heightened stress responses.
📏 Physical development concerns: Research also found shorter height and a greater risk of obesity in preschoolers whose mothers experienced untreated PPD.
Apart from these, PPD is associated with feeding problems and poor sleep routines in infants.
And as we mentioned earlier, children born to mothers with untreated perinatal depression are at greater risk for cognitive, emotional, verbal, and social developmental delays. The early years are crucial, and a parent's mental health plays a big role in shaping a child’s well-being.
💛 The good news? When mothers get the help they need, it creates a healthier environment for the baby too. Healing the parent helps heal the child.
🧠 What Happens if Postpartum Depression Is Not Treated?
Postpartum depression (PPD) is more than just a phase. When left unaddressed, it can spiral into long-lasting emotional, physical, and relational challenges for both the mother and the baby.
🌫️ Chronic Depression: Untreated PPD can persist beyond the postpartum period and evolve into long-term depressive disorders, affecting day-to-day functioning.
🪞 Impacts on Self-Esteem & Caregiving: Mothers often struggle with feelings of failure, guilt, or emotional numbness, making it harder to bond with or care for their child.
🧍♂️ Relationship Strain: The emotional toll can disrupt marital or family dynamics, increasing feelings of loneliness and misunderstanding.
🚨 Self-Harm & Suicide Risk: In severe cases, PPD increases the risk of self-harm or suicidal thoughts - making early support crucial, not optional.
🧸 Impact on the Baby: Babies of mothers with untreated PPD may experience emotional neglect, disrupted bonding, and developmental delays due to the mother’s dissociation or emotional withdrawal.
🔬 A review of 122 global studies found that untreated PPD has consequences on:
The mother’s physical health, psychological well being, relationships, and likelihood of risky behaviors.
The baby’s physical growth, sleep patterns, and emotional, cognitive, and social development.
Mother - child interactions, including quality of bonding, ability to breastfeed, and confidence in caregiving roles.
📊 How Common Is PPD in India?
Postpartum depression is shockingly common - but rarely spoken about. We referenced a study earlier that put PPD’s prevalence among Indian mothers at 26.3%; but according to another study, the overall prevalence of PPD in India is 22%, with notable regional differences:
South India: 26%
North India: 15%
🧭 In urban Pune alone, the prevalence was found to be as high as 26%.
But numbers only tell part of the story.
Despite these figures, PPD remains vastly underreported in India.
🤫 Cultural silence and stigma around mental health often stop mothers from opening up.
🧓 Societal expectations of being the "perfect mother" add pressure and guilt.
🏥 Limited mental health resources, especially in rural areas, make access to timely care difficult.
🧡 If you or someone you know is navigating early motherhood and recognizing signs of emotional distress or high risk for PPD, know this:
You are not alone, and support is available. Elfina offers culturally sensitive, accessible, and confidential mental health support tailored to new mothers across India.
💬 How Therapy Helps with Postpartum Depression
Therapy isn’t just about talking - it’s about healing, feeling seen, and slowly reclaiming your sense of self during one of life’s most vulnerable transitions.
Several evidence-based therapies have been shown to significantly ease the emotional weight of postpartum depression (PPD), each offering a different lens of support:
🧠 Cognitive Behavioral Therapy (CBT)

CBT helps new mothers reframe negative thoughts, challenge unhelpful beliefs, and build healthier emotional responses.
It’s especially effective in addressing the feelings of guilt, failure, or hopelessness that often accompany PPD.
Research shows that CBT significantly reduces symptoms of depression and anxiety in postpartum women, even over the long term.
It can be adapted for different formats - in-person, online, or even over the phone - making it flexible for busy, sleep-deprived moms.
🧍♀️ Interpersonal Therapy (IPT)

Motherhood often shifts the dynamic of personal relationships - and that’s where IPT steps in.
This therapy focuses on strengthening social connections, managing role transitions, and navigating conflicts or grief (like loss of identity or strained partner relationships).
It’s especially helpful for women who feel isolated, misunderstood, or overwhelmed by changing responsibilities.
It is considered a first-line, empirically validated treatment for postpartum depression, especially for breastfeeding women
Group IPT can also provide a sense of shared experience and support.
💥 Trauma-Informed Therapy

For many women, the postpartum period may awaken past trauma - or be traumatic in itself, especially in cases of difficult childbirth, medical complications, or loss.
A trauma-informed approach prioritizes safety, sensitivity, and trust.
It recognizes how past trauma can shape postpartum experiences and ensures that therapy does not retraumatize, but rather helps you process and move forward gently.
🧘♀️ Mindfulness-Based Therapy

Mindfulness-based techniques teach mothers to anchor themselves in the present, develop self-compassion, and ride the emotional waves without judgment.
These practices are especially helpful in calming the mind, easing anxiety, and promoting emotional regulation - all while building a nurturing space within.
💛 Therapy Through Elfina
Every mother deserves support - without shame, without travel, and without judgment.
Elfina connects mothers with compassionate therapists who specialize in perinatal and postpartum mental health - offering personalized, culturally sensitive care from the comfort of your home. Whether you're navigating sadness, anxiety, or emotional overwhelm, Elfina’s experts are here to help you feel seen, supported, and gently guided toward recovery.
🌿 Home Remedies for Emotional Support - Alongside Therapy

While therapy remains the most effective way to treat postpartum depression, small, consistent habits at home can nurture your mental well-being and support your healing journey.
Here are some gentle, evidence-backed ways to care for yourself:
🕰️ Build a Daily Rhythm
Creating a predictable routine - even if it’s just a morning shower or afternoon tea - helps anchor your day. Prioritizing small self-care rituals can calm the mind and reduce overwhelm.
👭 Stay Connected
Talk to a friend. Join a new moms’ group online or in person. Even a short check-in with someone who gets it can ease feelings of isolation and remind you that you're not alone in this.
🧘 Mindfulness & Movement
Short walks in fresh air, mindful breathing, or guided meditations can help reduce anxiety and re-center your thoughts. Gentle movement helps release mood-boosting endorphins - no gym required.
🥗 Nutritional Nourishment
Omega-3 fatty acids (EPA and DHA) - often found in flaxseeds, walnuts, and fatty fish - may lower the risk and severity of postpartum depression.
Iron, calcium, and vitamin-rich foods also support energy levels and mood stability, especially while breastfeeding. Don’t forget hydration!
The American Pregnancy Association notes that Omega-3s may reduce the risk of PPD, and Nebraska Medicine recommends iron and nutrient support for breastfeeding mothers.
🖋️ Journal or Create
Sometimes, the best release is through expression. Writing your thoughts, drawing, or simply doodling can help externalize worries and reconnect you with yourself.
💗 Remember, these practices aren’t meant to replace therapy - but to complement your healing. They’re small steps with big emotional payoffs.
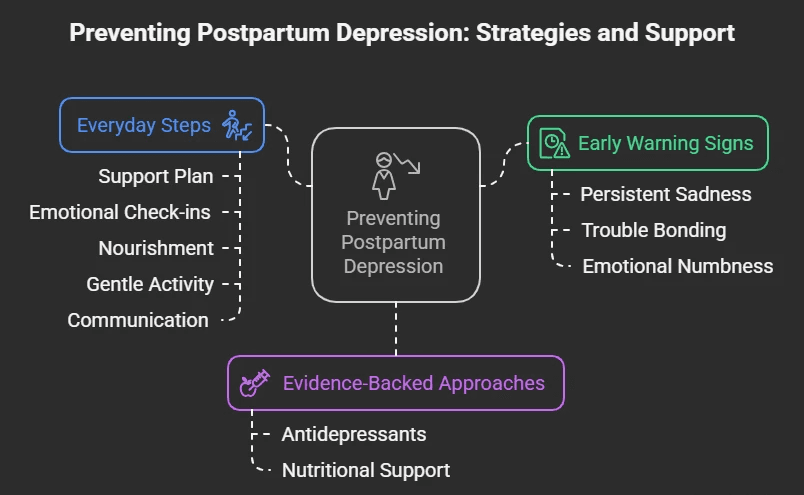
🌼 Can You Prevent Postpartum Depression?
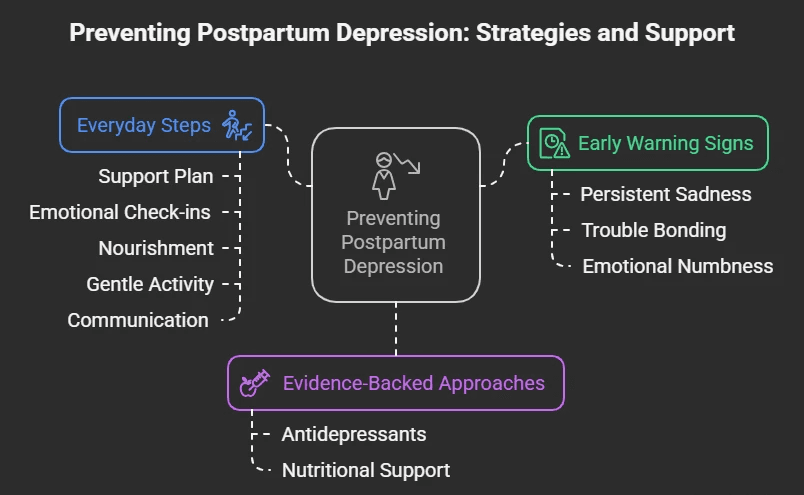
Postpartum depression isn’t entirely preventable - but knowing your risk factors, preparing proactively, and seeking early support can make a real difference.
🔍 Know the Early Warning Signs
Understanding what to watch for helps you take action before symptoms deepen. Be mindful of:
Persistent sadness or anxiety
Trouble bonding with your baby
Guilt, hopelessness, or feeling emotionally “numb”
Loss of interest in activities or relationships
Sleep or appetite changes unrelated to baby care
If these signs last more than two weeks, it’s time to seek help - you don’t need to wait for things to get worse.
🧬 Evidence-Backed Preventive Approaches
An Australian review found that biological interventions - including antidepressants (for high-risk individuals) and nutritional support - showed the strongest results in preventing postpartum depression.
You can speak to a doctor before delivery about your mental health history or vulnerabilities to explore proactive options, especially if you’ve had depression before.
💡 Everyday Steps That Help Build Resilience
You don’t have to wait for a diagnosis to start protecting your mental wellbeing. Small changes can go a long way:
Create a postpartum support plan: Line up help from family, friends, or professionals.
Practice daily emotional check-ins: Reflect, journal, or talk to someone you trust.
Focus on nourishment: Nutrients like omega-3s, iron, and Vitamin D support brain health.
Stay gently active: Short walks, deep breathing, or stretching can ease tension.
Communicate with your partner or loved ones: Let them know how you’re feeling, even if it’s messy or hard to explain.
Therapy during pregnancy: Talking to a therapist before symptoms arise can act as both prevention and preparation.
✨ Remember:
Seeking support early is not a sign of weakness - it’s one of the strongest things you can do for yourself and your baby. Elfina is here to walk with you through all stages - not just crisis.
You deserve care even before you think you need it.
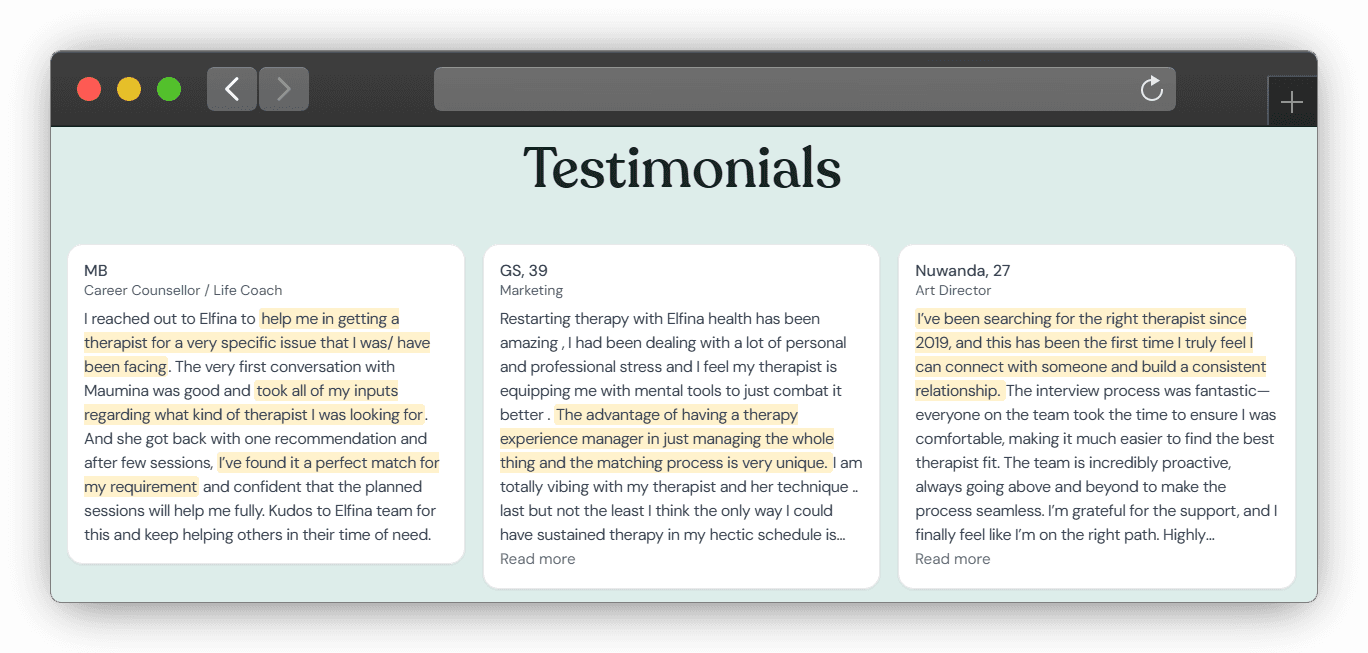
💛 How Elfina Helps With Postpartum Depression

When you’re navigating postpartum depression, the last thing you need is more overwhelm. Elfina makes your healing simpler, gentler, and truly supportive - every step of the way.
Here’s how we care for you:
🧠 Expert Therapists, Handpicked for You
Our therapists specialize in maternal mental health, trauma recovery, and emotional wellbeing during early motherhood.
They’re not just experienced - they’re deeply empathetic, trained to understand the unique challenges of postpartum life.
In fact, 80% of Elfina’s therapists have over 5 years of experience, with an average of 8 years in practice.
🎯 Personalized Therapy, Matched to Your Needs
No more trial-and-error. Our smart therapist-matching system connects you with someone who aligns with your emotional goals, therapy preferences (whether you prefer structured sessions or free-flowing chats), and support needs.
94% of clients find the right therapist on their first match.
🏡 Judgment-Free, Confidential Support - From Home
You don’t have to dress up or commute to get help. Elfina offers online therapy in a safe, non-judgmental space, so you can open up comfortably - even if the baby’s asleep in the next room.
⏰ Flexible Scheduling That Understands Motherhood
We know your time isn’t your own right now. Elfina offers flexible sessions, so you can get help when it fits - during naptime, after bedtime, or whenever you can catch a breath.
🤝 Continuous Guidance Throughout Your Journey
You’re never alone. From booking to progress check-ins, our Therapy Experience Manager (TEM) walks with you to make sure your experience feels aligned, effective, and evolving with your needs.
✨ Because when mothers are supported, families thrive.
Elfina’s here to make sure your postpartum healing feels personal, compassionate, and empowering - just like it should.
Book your first session today - and take the first step toward feeling like yourself again.
💙 Conclusion
Postpartum Depression is not a personal failure - it’s a medical condition. And it’s treatable.
If you’re struggling, know this: you are not alone. So many mothers quietly carry the weight of postpartum depression, thinking they have to push through it on their own. You don’t.
You don’t have to wait for things to get worse to ask for help.
You deserve support - early, gentle, and personalized.
Elfina’s online therapy connects you with compassionate, expert therapists trained in maternal mental health. From the comfort of your home, you can begin to process your emotions, rebuild your confidence, and reclaim your joy, your strength, and your bond with your baby.
🌷 Your healing matters - for you, and for your baby.
Other blogs
Postpartum Depression: What New Mothers in India Need to Know
May 12, 2025
|
18
min read
|
Tanvi

The Other Side of Motherhood
Motherhood is often celebrated as a time of unmatched joy and fulfillment. From baby showers to blessings, the arrival of a newborn is expected to bring happiness. But for many mothers, especially in the weeks and months following childbirth, this period is marked not by joy - but by overwhelming sadness, anxiety, and emotional exhaustion.
This emotional struggle has a name: Postpartum Depression (PPD).
According to the American Psychological Association (APA), postpartum depression is a serious mental health condition that can occur days, weeks, or even months after childbirth, and if left untreated, may last for many weeks or months. It goes far beyond the “baby blues,” affecting a mother’s mood, energy, and ability to care for herself or her baby.
In India, postpartum depression is far more common than many realize. A study by Lanjewar, Shraddha et al. found that 26.3% of Indian mothers experience symptoms of depression after delivery. Despite this high number, cultural stigma, lack of awareness, and limited access to mental health care often prevent mothers from speaking up or seeking help.
What’s more alarming is that for 36% of mothers who experience mental health challenges soon after childbirth, symptoms can persist for as long as 18 months - and in some cases, up to two years. These extended struggles can deeply impact not only the mother’s well-being but also her relationship with her baby, her partner, and herself.
The good news? Postpartum depression is treatable. With the right support, healing is possible.
This blog is here to break the silence. We’ll help you understand what PPD is, how it differs from the baby blues, what signs to look out for, and most importantly - how compassionate, expert-led care like the kind offered by Elfina Health can make a real difference.
Perinatal vs Postpartum Depression vs Prenatal Depression
Motherhood is often described as a beautiful journey - but for many women, it can come with emotional storms that are difficult to explain or share. Understanding the terms used to describe mental health conditions around childbirth is an important first step in recognizing and seeking help.
Perinatal depression is a broad term that includes both prenatal depression (depression during pregnancy) and postpartum depression (depression after childbirth). While the experiences overlap, each phase comes with its own emotional, physical, and psychological challenges.
Definitions and Differences
Term | Timing | Description |
Perinatal Depression | During pregnancy and up to 1 year after birth | An umbrella term for mood disorders before and after childbirth. |
Prenatal Depression | During pregnancy | Depression that occurs during pregnancy - often marked by sadness, fear, or exhaustion. |
Postpartum Depression | After childbirth (typically within 4 weeks to 1 year) | Depression that follows childbirth; more persistent and intense than the "baby blues". |
While these conditions differ in timing, they often share common symptoms like deep sadness, irritability, anxiety, disrupted sleep, and changes in appetite. Unfortunately, they’re frequently overlooked or misunderstood - especially in India - due to social stigma and a lack of mental health awareness.
What Happens During Perinatal Depression?
Perinatal depression is more than just feeling overwhelmed - it's a serious and often misunderstood medical condition. It can affect a mother during pregnancy (prenatal) or after delivery (postpartum), showing up as intense sadness, detachment, anxiety, and drastic changes in energy, appetite, or sleep patterns.
In the case of postpartum depression (PPD), symptoms often appear between the second and sixth week after childbirth, but can develop any time within the first year. While many new mothers experience what’s commonly called the “baby blues,” postpartum depression goes far deeper and lasts much longer. It may involve constant low mood, hopelessness, tearfulness, and even disturbing thoughts - such as excessive worries about the baby's health, feelings of worthlessness, or in extreme cases, suicidal ideation or thoughts of harming the child. These are deeply distressing experiences, and contrary to common belief, they are not signs of being a “bad mother”.
Perinatal depression affects more than just the mother’s mood. It can interfere with her ability to bond with her baby, leading to emotional distance or feelings of guilt and disconnection. According to the APA, perinatal depression can contribute to sleep and feeding difficulties in the baby, creating a stressful environment for both mother and child.
The ripple effects of perinatal depression can be long-term, especially for the child. Research shows that children born to mothers with untreated perinatal depression are at greater risk for cognitive, emotional, verbal, and social developmental delays. Emotional availability in those early stages is crucial for a child’s growth, and when maternal mental health suffers, it can impact the child’s emotional security, attachment, and ability to regulate emotions. These outcomes are not signs of poor parenting - they are the result of an untreated medical condition that deserves timely recognition, compassion, and support.
The good news is that perinatal and postpartum depression are treatable. With the right help - whether through therapy, support groups, medical guidance, or simply being heard - recovery is entirely possible. Early intervention doesn’t just help the mother heal; it also lays a stronger emotional foundation for the child.
Recognizing the Symptoms of Postpartum Depression
Postpartum Depression doesn’t always look the same for every mother - but it’s more than just feeling tired or overwhelmed. It can manifest emotionally, physically, and behaviorally, often lasting for weeks or even months if left unaddressed.
According to the U.S. National Institute of Mental Health, common symptoms include:
Persistent sadness, anxiety, or a sense of emotional numbness
Many mothers report feeling hopeless or emotionally disconnected most of the day, nearly every day.Loss of interest or joy in activities
This includes disinterest in the baby or things that once brought happiness.Feelings of guilt, worthlessness, or inadequacy
Mothers may blame themselves unnecessarily or feel like they’re failing, even when they’re doing their best.Irritability, restlessness, or frequent frustration
Small things may trigger intense emotions or sudden outbursts.Excessive worry or panic attacks
These may include racing thoughts, heart palpitations, or overwhelming anxiety about the baby’s safety or one’s ability to care for them.Difficulty concentrating or making decisions
A foggy mind or forgetfulness can interfere with daily tasks and responsibilities.Changes in sleep and appetite
This might include insomnia despite exhaustion, sleeping too much, loss of appetite, or overeating.Physical symptoms without a clear cause
Aches, pains, headaches, or digestive issues that don’t respond to usual treatment can be signs.Trouble bonding with the baby
Some mothers feel detached or worry that they aren’t connecting emotionally with their child.Thoughts of self-harm or harming the baby (in severe cases)
These intrusive thoughts can be deeply distressing and are a clear sign to seek immediate professional support.
If you notice these symptoms persisting for more than two weeks, it's important to seek professional help. Postpartum depression is not a personal weakness - it's a medical condition, and with the right support, it can be treated.
Elfina offers confidential, culturally sensitive online counseling tailored for new and expecting mothers.
Baby Blues vs Postpartum Depression vs Postpartum Psychosis
Baby Blues
According to the South Dakota Department of Health, it affects around 70 - 80% of new mothers, often within the first few days after childbirth. Symptoms include mood swings, tearfulness, irritability, and anxiety. These emotional ups and downs are usually mild and tend to resolve on their own within two weeks without medical treatment.
Postpartum Depression (PPD)
Unlike the baby blues, PPD is more intense and long-lasting. It can begin anytime within the first year after delivery, often requiring professional support. Mothers may experience overwhelming sadness, fatigue, hopelessness, loss of interest in the baby, and even thoughts of self-harm. It affects daily functioning and emotional connection with the baby - but it is treatable with the right care.
Postpartum Psychosis
A rare but severe condition, postpartum psychosis is a psychiatric emergency that usually develops within the first few days to weeks after childbirth. Symptoms may include hallucinations, delusions, extreme confusion, and disorganized behavior. Immediate medical intervention is critical.
Certain factors such as advanced maternal age and low birth weight (under 1500 grams) are potential contributors, while high birth weight (over 4500 grams) and maternal diabetes may offer some protective effect for first-time mothers within the first 90 days.
Edinburgh Postnatal Depression Scale (EPDS)
The Edinburgh Postnatal Depression Scale (EPDS) is a widely used screening tool designed to help healthcare providers identify mothers who may be experiencing postpartum depression (PPD). It consists of 10 simple, self-reported questions that focus on the emotional state of new mothers, helping to assess feelings such as sadness, hopelessness, and anxiety over the previous week.
For further credibility, you can refer to the full citation:
Cox, J L et al. “Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale.” The British journal of psychiatry : the journal of mental science vol. 150 (1987): 782-6. doi: 10.1192/bjp.150.6.782
We’ve listed the questions below along with the scoring scale to help you evaluate your emotional well-being. It’s important to answer honestly, as this will help determine if you may need further support or intervention.
EDPS Questionnaire
I have been able to laugh and see the funny side of things
0 = As much as I always could
1 = Not quite so much now
2 = Definitely not so much now
3 = Not at all
I have looked forward with enjoyment to things
0 = As much as I ever did
1 = Rather less than I used to
2 = Definitely less than I used to
3 = Hardly at all
I have blamed myself unnecessarily when things went wrong
0 = No, never
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
I have been anxious or worried for no good reason
0 = No, not at all
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
I have felt scared or panicked for no good reason
0 = No, not at all
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
Things have been getting on top of me
0 = No, never
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
I have been so unhappy that I have had difficulty sleeping
0 = No, never
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, most of the time
I have felt sad or miserable
0 = No, never
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
I have been so unhappy that I have been crying
0 = No, never
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
The thought of harming myself has occurred to me
0 = No, never
1 = Hardly ever
2 = Yes, sometimes
3 = Yes, very often
📊 EPDS Scoring Guide
Here’s the EDPS Scoring Guide as per COPE (Centre of Perinatal Excellence):
🔢 Total Score:
13 or more → 🟠 Possible Depressive Symptoms
This score signals the need for follow-up.
Antenatal period: Repeat the EPDS in 2–4 weeks. If the second score remains ≥13, refer to an appropriate health professional, preferably the woman's general practitioner.
Postnatal period: Consider referral or continued care based on clinical judgment.
💬 Questions 3, 4, and 5 → ⚠️ Monitor for Anxiety
Even if the total score is below 13, elevated responses on these questions may indicate anxiety symptoms requiring follow-up.
🔴 Question 10 (Self-harm)
If the response is 1, 2, or 3, it’s critical to assess the safety of the woman and any children in her care. Seek urgent advice and/or arrange a mental health assessment based on clinical judgment.
🧠 What Causes Postpartum Depression (PPD)?
Postpartum Depression (PPD) doesn’t stem from a single cause - it’s the result of a complex interplay between hormonal, emotional, physical, and environmental factors. While every new parent’s journey is different, certain experiences and conditions can significantly increase the risk.
🔄 Hormonal Fluctuations
After childbirth, estrogen and progesterone levels - which were elevated throughout pregnancy - drop sharply. These rapid hormonal shifts can impact brain chemistry and trigger mood disturbances, especially in individuals already sensitive to such changes.
😴 Sleep Deprivation & Physical Exhaustion
Caring for a newborn often means interrupted or inadequate sleep, which can compound physical fatigue and emotional instability. Prolonged exhaustion not only affects mood but also limits one’s ability to cope with daily stressors, increasing vulnerability to depression.
💔 Lack of Emotional or Social Support
Feeling unsupported - whether by a partner, family, friends, or community - can deepen feelings of isolation, inadequacy, or helplessness. Emotional availability from others plays a crucial role in helping new parents adjust and feel seen during this transition.
🚨 Traumatic Childbirth
Difficult or traumatic birth experiences - such as emergency C-sections, excessive pain, complications, or feeling a loss of control - can have lingering psychological effects. These may include flashbacks, heightened anxiety, and an increased risk of PPD, anxiety disorders, or even postpartum psychosis.
🤰 Unplanned or Unintended Pregnancy
Pregnancies that were unplanned - even if not unwelcome - can contribute to emotional conflict, stress, or ambivalence. These feelings may intensify postpartum, especially in the absence of adequate preparation or support.
🌀 Psychosocial Stressors
The postpartum period is filled with new challenges: identity shifts, physical recovery, lifestyle changes, financial strain, and a redefinition of relationships. When these are combined with unrealistic societal expectations or self-imposed pressure to "bounce back", it can create a perfect storm for emotional burnout.
Even though these causes may raise the risk, PPD can affect anyone - regardless of how “prepared” or “happy” they felt about the pregnancy. Recognizing these risk factors helps reduce stigma and encourages early, compassionate support.
⚠️ Risk Factors for Postpartum Depression
While anyone can experience PPD, certain circumstances may increase the likelihood of its onset. These risk factors span physical, psychological, cultural, and environmental domains:
👶 First-Time Motherhood
Navigating the unknowns of parenting for the first time can bring anxiety, insecurity, and overwhelming responsibility - especially without prior experience or adequate guidance.
🧠 Personal or Family History of Mental Illness
Individuals with a history of depression, anxiety, bipolar disorder, or schizophrenia - or those with close family members who’ve experienced such conditions - are at a higher risk for developing PPD.
💔 Financial, Relationship, or Marital Stress
Tensions around money, unstable partnerships, or unresolved conflicts can place an emotional strain during what should be a time of recovery and bonding.
🏥 Birth or Breastfeeding Complications
Experiencing a traumatic labor, emergency C-section, preterm delivery, difficulty breastfeeding, or a low-birth-weight baby can increase stress and feelings of inadequacy or failure.
🧍 Limited Social or Emotional Support
Lack of involvement or understanding from a partner, family, or community can intensify feelings of isolation - especially in cultures where motherhood is idealized and support is minimal.
🌙 Postpartum Sleep Disruption
Severe sleep deprivation or irregular sleep patterns during the postpartum period not only affect physical health but can dramatically worsen mood and cognitive functioning.
⚖️ Obesity and Nutritional Factors
Studies indicate a positive correlation between higher levels of obesity and PPD risk. Nutritional deficiencies - such as low Vitamin D or iron (postpartum anemia) - may also play a role.
🚼 Cultural Pressures and Gender Preference
In some societies, particularly in parts of Asia and Africa, giving birth to a female child may lead to social pressure or disappointment, exacerbating emotional distress for new mothers.
🧍♀️ Multiple Births or Preterm Infants
Managing twins or more, or caring for premature or medically fragile babies, requires heightened attention and resources - often leading to exhaustion and emotional strain.
💬 If you recognize yourself in any of these risk factors or feel overwhelmed during your postpartum journey, know that you're not alone. Early awareness can make a world of difference. At Elfina, our experts are here to support you with compassionate, culturally sensitive, and evidence-based guidance. Whether it’s your first baby or not, reaching out for help is a powerful act of care - for yourself and your child.
🧡 Don’t wait for things to get worse - connect with Elfina early for personalized support.
Can Postpartum Depression Affect the Baby?
The U.S. Office on Women’s Health compiled leading research on how postpartum depression (PPD) can affect babies - and the findings show it can have a real and lasting impact if left untreated:
🧸 Bonding issues: PPD can make it difficult for mothers to connect emotionally with their babies, leading to attachment problems.
😢 Increased crying and agitation: Babies may cry more often and seem harder to soothe.
🧠 Delays in language and learning: Children may take longer to start speaking or have trouble with early learning.
🚸 Behavioral problems: These can include trouble adjusting to school or new environments, as well as heightened stress responses.
📏 Physical development concerns: Research also found shorter height and a greater risk of obesity in preschoolers whose mothers experienced untreated PPD.
Apart from these, PPD is associated with feeding problems and poor sleep routines in infants.
And as we mentioned earlier, children born to mothers with untreated perinatal depression are at greater risk for cognitive, emotional, verbal, and social developmental delays. The early years are crucial, and a parent's mental health plays a big role in shaping a child’s well-being.
💛 The good news? When mothers get the help they need, it creates a healthier environment for the baby too. Healing the parent helps heal the child.
🧠 What Happens if Postpartum Depression Is Not Treated?
Postpartum depression (PPD) is more than just a phase. When left unaddressed, it can spiral into long-lasting emotional, physical, and relational challenges for both the mother and the baby.
🌫️ Chronic Depression: Untreated PPD can persist beyond the postpartum period and evolve into long-term depressive disorders, affecting day-to-day functioning.
🪞 Impacts on Self-Esteem & Caregiving: Mothers often struggle with feelings of failure, guilt, or emotional numbness, making it harder to bond with or care for their child.
🧍♂️ Relationship Strain: The emotional toll can disrupt marital or family dynamics, increasing feelings of loneliness and misunderstanding.
🚨 Self-Harm & Suicide Risk: In severe cases, PPD increases the risk of self-harm or suicidal thoughts - making early support crucial, not optional.
🧸 Impact on the Baby: Babies of mothers with untreated PPD may experience emotional neglect, disrupted bonding, and developmental delays due to the mother’s dissociation or emotional withdrawal.
🔬 A review of 122 global studies found that untreated PPD has consequences on:
The mother’s physical health, psychological well being, relationships, and likelihood of risky behaviors.
The baby’s physical growth, sleep patterns, and emotional, cognitive, and social development.
Mother - child interactions, including quality of bonding, ability to breastfeed, and confidence in caregiving roles.
📊 How Common Is PPD in India?
Postpartum depression is shockingly common - but rarely spoken about. We referenced a study earlier that put PPD’s prevalence among Indian mothers at 26.3%; but according to another study, the overall prevalence of PPD in India is 22%, with notable regional differences:
South India: 26%
North India: 15%
🧭 In urban Pune alone, the prevalence was found to be as high as 26%.
But numbers only tell part of the story.
Despite these figures, PPD remains vastly underreported in India.
🤫 Cultural silence and stigma around mental health often stop mothers from opening up.
🧓 Societal expectations of being the "perfect mother" add pressure and guilt.
🏥 Limited mental health resources, especially in rural areas, make access to timely care difficult.
🧡 If you or someone you know is navigating early motherhood and recognizing signs of emotional distress or high risk for PPD, know this:
You are not alone, and support is available. Elfina offers culturally sensitive, accessible, and confidential mental health support tailored to new mothers across India.
💬 How Therapy Helps with Postpartum Depression
Therapy isn’t just about talking - it’s about healing, feeling seen, and slowly reclaiming your sense of self during one of life’s most vulnerable transitions.
Several evidence-based therapies have been shown to significantly ease the emotional weight of postpartum depression (PPD), each offering a different lens of support:
🧠 Cognitive Behavioral Therapy (CBT)

CBT helps new mothers reframe negative thoughts, challenge unhelpful beliefs, and build healthier emotional responses.
It’s especially effective in addressing the feelings of guilt, failure, or hopelessness that often accompany PPD.
Research shows that CBT significantly reduces symptoms of depression and anxiety in postpartum women, even over the long term.
It can be adapted for different formats - in-person, online, or even over the phone - making it flexible for busy, sleep-deprived moms.
🧍♀️ Interpersonal Therapy (IPT)

Motherhood often shifts the dynamic of personal relationships - and that’s where IPT steps in.
This therapy focuses on strengthening social connections, managing role transitions, and navigating conflicts or grief (like loss of identity or strained partner relationships).
It’s especially helpful for women who feel isolated, misunderstood, or overwhelmed by changing responsibilities.
It is considered a first-line, empirically validated treatment for postpartum depression, especially for breastfeeding women
Group IPT can also provide a sense of shared experience and support.
💥 Trauma-Informed Therapy

For many women, the postpartum period may awaken past trauma - or be traumatic in itself, especially in cases of difficult childbirth, medical complications, or loss.
A trauma-informed approach prioritizes safety, sensitivity, and trust.
It recognizes how past trauma can shape postpartum experiences and ensures that therapy does not retraumatize, but rather helps you process and move forward gently.
🧘♀️ Mindfulness-Based Therapy

Mindfulness-based techniques teach mothers to anchor themselves in the present, develop self-compassion, and ride the emotional waves without judgment.
These practices are especially helpful in calming the mind, easing anxiety, and promoting emotional regulation - all while building a nurturing space within.
💛 Therapy Through Elfina
Every mother deserves support - without shame, without travel, and without judgment.
Elfina connects mothers with compassionate therapists who specialize in perinatal and postpartum mental health - offering personalized, culturally sensitive care from the comfort of your home. Whether you're navigating sadness, anxiety, or emotional overwhelm, Elfina’s experts are here to help you feel seen, supported, and gently guided toward recovery.
🌿 Home Remedies for Emotional Support - Alongside Therapy

While therapy remains the most effective way to treat postpartum depression, small, consistent habits at home can nurture your mental well-being and support your healing journey.
Here are some gentle, evidence-backed ways to care for yourself:
🕰️ Build a Daily Rhythm
Creating a predictable routine - even if it’s just a morning shower or afternoon tea - helps anchor your day. Prioritizing small self-care rituals can calm the mind and reduce overwhelm.
👭 Stay Connected
Talk to a friend. Join a new moms’ group online or in person. Even a short check-in with someone who gets it can ease feelings of isolation and remind you that you're not alone in this.
🧘 Mindfulness & Movement
Short walks in fresh air, mindful breathing, or guided meditations can help reduce anxiety and re-center your thoughts. Gentle movement helps release mood-boosting endorphins - no gym required.
🥗 Nutritional Nourishment
Omega-3 fatty acids (EPA and DHA) - often found in flaxseeds, walnuts, and fatty fish - may lower the risk and severity of postpartum depression.
Iron, calcium, and vitamin-rich foods also support energy levels and mood stability, especially while breastfeeding. Don’t forget hydration!
The American Pregnancy Association notes that Omega-3s may reduce the risk of PPD, and Nebraska Medicine recommends iron and nutrient support for breastfeeding mothers.
🖋️ Journal or Create
Sometimes, the best release is through expression. Writing your thoughts, drawing, or simply doodling can help externalize worries and reconnect you with yourself.
💗 Remember, these practices aren’t meant to replace therapy - but to complement your healing. They’re small steps with big emotional payoffs.
🌼 Can You Prevent Postpartum Depression?
Postpartum depression isn’t entirely preventable - but knowing your risk factors, preparing proactively, and seeking early support can make a real difference.
🔍 Know the Early Warning Signs
Understanding what to watch for helps you take action before symptoms deepen. Be mindful of:
Persistent sadness or anxiety
Trouble bonding with your baby
Guilt, hopelessness, or feeling emotionally “numb”
Loss of interest in activities or relationships
Sleep or appetite changes unrelated to baby care
If these signs last more than two weeks, it’s time to seek help - you don’t need to wait for things to get worse.
🧬 Evidence-Backed Preventive Approaches
An Australian review found that biological interventions - including antidepressants (for high-risk individuals) and nutritional support - showed the strongest results in preventing postpartum depression.
You can speak to a doctor before delivery about your mental health history or vulnerabilities to explore proactive options, especially if you’ve had depression before.
💡 Everyday Steps That Help Build Resilience
You don’t have to wait for a diagnosis to start protecting your mental wellbeing. Small changes can go a long way:
Create a postpartum support plan: Line up help from family, friends, or professionals.
Practice daily emotional check-ins: Reflect, journal, or talk to someone you trust.
Focus on nourishment: Nutrients like omega-3s, iron, and Vitamin D support brain health.
Stay gently active: Short walks, deep breathing, or stretching can ease tension.
Communicate with your partner or loved ones: Let them know how you’re feeling, even if it’s messy or hard to explain.
Therapy during pregnancy: Talking to a therapist before symptoms arise can act as both prevention and preparation.
✨ Remember:
Seeking support early is not a sign of weakness - it’s one of the strongest things you can do for yourself and your baby. Elfina is here to walk with you through all stages - not just crisis.
You deserve care even before you think you need it.
💛 How Elfina Helps With Postpartum Depression

When you’re navigating postpartum depression, the last thing you need is more overwhelm. Elfina makes your healing simpler, gentler, and truly supportive - every step of the way.
Here’s how we care for you:
🧠 Expert Therapists, Handpicked for You
Our therapists specialize in maternal mental health, trauma recovery, and emotional wellbeing during early motherhood.
They’re not just experienced - they’re deeply empathetic, trained to understand the unique challenges of postpartum life.
In fact, 80% of Elfina’s therapists have over 5 years of experience, with an average of 8 years in practice.
🎯 Personalized Therapy, Matched to Your Needs
No more trial-and-error. Our smart therapist-matching system connects you with someone who aligns with your emotional goals, therapy preferences (whether you prefer structured sessions or free-flowing chats), and support needs.
94% of clients find the right therapist on their first match.
🏡 Judgment-Free, Confidential Support - From Home
You don’t have to dress up or commute to get help. Elfina offers online therapy in a safe, non-judgmental space, so you can open up comfortably - even if the baby’s asleep in the next room.
⏰ Flexible Scheduling That Understands Motherhood
We know your time isn’t your own right now. Elfina offers flexible sessions, so you can get help when it fits - during naptime, after bedtime, or whenever you can catch a breath.
🤝 Continuous Guidance Throughout Your Journey
You’re never alone. From booking to progress check-ins, our Therapy Experience Manager (TEM) walks with you to make sure your experience feels aligned, effective, and evolving with your needs.
✨ Because when mothers are supported, families thrive.
Elfina’s here to make sure your postpartum healing feels personal, compassionate, and empowering - just like it should.
Book your first session today - and take the first step toward feeling like yourself again.
💙 Conclusion
Postpartum Depression is not a personal failure - it’s a medical condition. And it’s treatable.
If you’re struggling, know this: you are not alone. So many mothers quietly carry the weight of postpartum depression, thinking they have to push through it on their own. You don’t.
You don’t have to wait for things to get worse to ask for help.
You deserve support - early, gentle, and personalized.
Elfina’s online therapy connects you with compassionate, expert therapists trained in maternal mental health. From the comfort of your home, you can begin to process your emotions, rebuild your confidence, and reclaim your joy, your strength, and your bond with your baby.
🌷 Your healing matters - for you, and for your baby.
Other blogs
Frequently Asked Questions
What types of therapy do you offer?
Can I meet my therapist in-person?
How do you match me with a therapist?
How much does therapy cost?
Do you offer free trials?
Finding The Right Fit, Made Easy
© Mindaro Health Technologies. All rights reserved
© Mindaro Health Technologies. All rights reserved
Finding the right fit, made easy.
FAQs
What types of therapy do you offer?
What types of therapy do you offer?
Can I meet my therapist in-person?
Can I meet my therapist in-person?
How do you match me with a therapist?
How do you match me with a therapist?
How much does therapy cost?
How much does therapy cost?
Do you offer free trials?
Do you offer free trials?







